A new study shows that AI can spot hidden signs in mammograms years before breast cancer develops, offering hope for tailored screening and earlier, life-saving action.
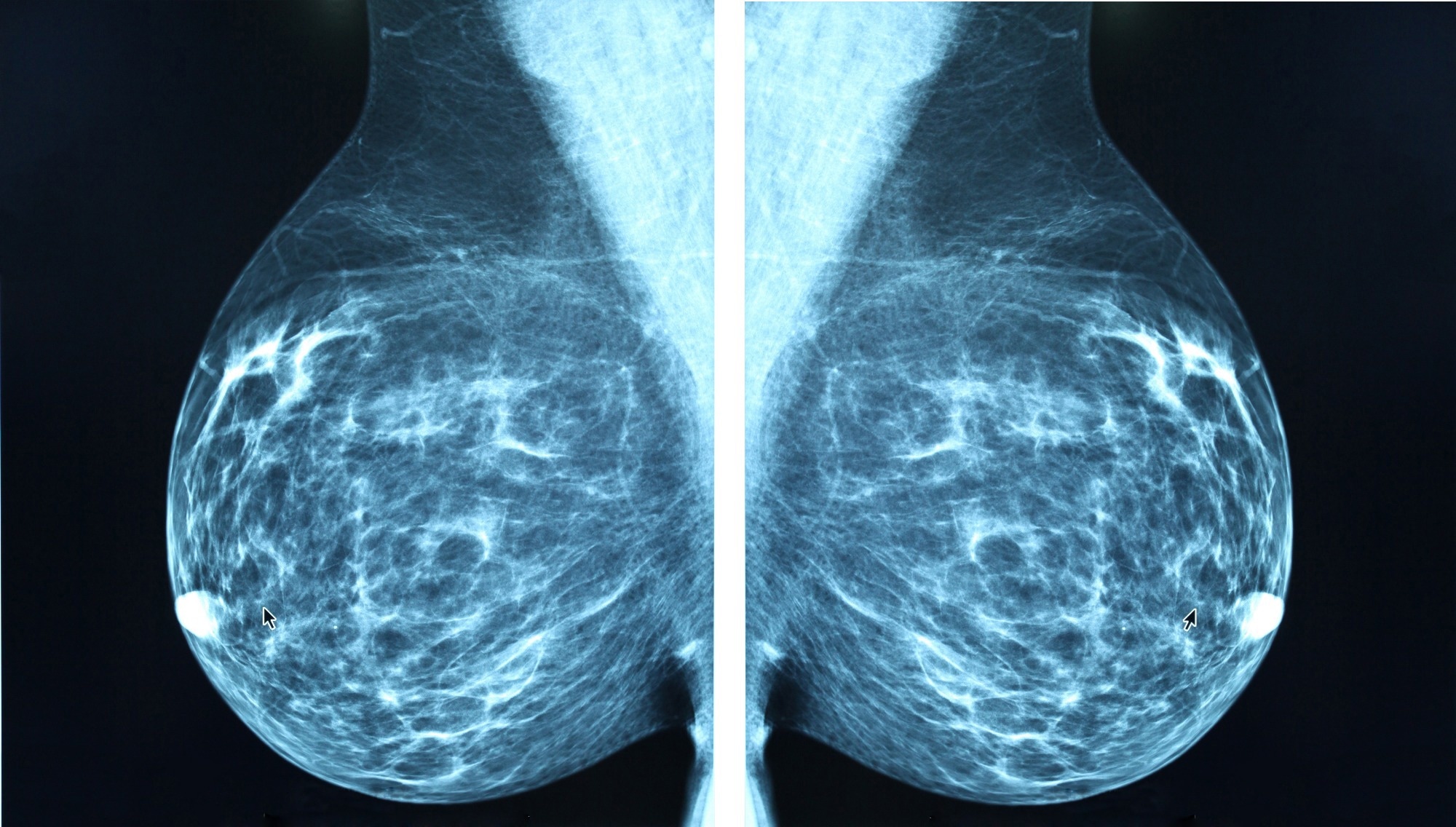 Study: Artificial Intelligence Algorithm for Subclinical Breast Cancer Detection. Image Credit: Blue Planet Earth / Shutterstock
Study: Artificial Intelligence Algorithm for Subclinical Breast Cancer Detection. Image Credit: Blue Planet Earth / Shutterstock
In a recent study published in the JAMA Network Open, researchers evaluated whether a commercial artificial intelligence (AI) tool, originally developed for breast cancer detection, could leverage screening mammograms to estimate the risk of future breast cancer development years before clinical diagnosis. They used a cohort study comprising almost 350,000 screening examinations from 116,495 women to generate AI-based cancer detection scores, which were assessed as proxies for subsequent breast cancer risk rather than for direct diagnosis.
Study findings revealed that the AI algorithm assigned higher cancer detection scores to breasts that would later develop breast cancer, even 4–6 years before clinical diagnosis, compared to breasts that did not develop cancer. This suggests that commercial AI tools may help identify women at higher risk of developing breast cancer well in advance of diagnosis, providing a pathway for more personalized risk-based screening and earlier intervention.
Background
Breast cancer is the most commonly diagnosed cancer among women, accounting for almost 25% of all female malignancies (2.3 million new cases, 2022) and more than 670,000 deaths annually. Routine mammography-based screening represents the first line of defense against breast cancer-associated morbidity and mortality, substantially improving patient survival rates by the early detection of malignancies and their subsequent timely treatment.
Unfortunately, conventional mammography screening methodologies are prone to accuracy and reliability confounds, relying heavily on the subjective expertise of human reviewers (radiologists). Furthermore, traditional screening techniques fail to identify breast cancer malignancies that develop between screenings, resulting in detection delays and their associated clinical and socioeconomic demerits.
Recent advances in commercial artificial intelligence (AI) tools have enabled the generation of radiologist-aided breast and examination-level neoplasm scores, utilizing minute variations in mammograms to help clinicians assess breast cancer risk earlier and with greater accuracy.
While previous studies hypothesized that AI could use subclinical mammography features to predict future breast cancer incidence, this large-scale study scientifically evaluated that hypothesis using a national screening program cohort.
About the study
The present study assessed the predictive accuracy, overall performance, and reliability of a commercial AI tool in estimating future breast cancer risk from patient-derived mammogram data. The study employs a retrospective cohort design and adheres to the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines.
Study data were obtained from the Cancer Registry of Norway's BreastScreen Norway program, which comprises biennial digital mammography screening (mediolateral oblique [MLO] and craniocaudal [CC] projections) of more than 680,000 Norwegian women (aged 50-69 years) between 2004 and 2018. Participants were required to present at least three scans, each of which was independently evaluated using both traditional (radiologist double reading) and AI-based screening approaches.
The AI tool (INSIGHT MMG, version 1.1.7.2) used in this study was obtained in collaboration with Lunit Inc., however, the latter had no access to study data or influence over the methodologies or outcomes. The algorithm screens mammograms and provides a participant-specific continuous cancer detection score (range = 0-100) with higher values suggesting a higher breast cancer risk. The study compared these scores—including absolute differences between the two breasts—across successive mammograms and evaluated how these scores tracked with subsequent breast cancer diagnoses, in addition to comparisons with traditional radiologist evaluations.
Study findings
After excluding participants with incomplete data or insufficient mammograms and follow-up, data from 116,495 participants were subjected to subsequent analyses. Women who developed breast cancer had substantially higher mean AI scores and greater absolute differences in scores between breasts years before diagnosis compared to women who remained cancer-free. For example, among women who developed screening-detected cancer, the mean AI scores for the affected breast were 19.2, 30.8, and 82.7 across the first, second, and third study rounds, respectively. In contrast, healthy participants reported mean AI scores of 9.5, 8.2, and 5.0 across the same study rounds.
In contrast, women with no breast cancer diagnosis during the study period had mean AI scores of 7.1, 6.7, and 6.4, respectively. Sensitivity analyses confirmed these findings, highlighting the robustness of AI predictions. Importantly, the study authors note that these findings suggest AI tools may enable identification of women at increased risk 4–6 years before breast cancer diagnosis, allowing for consideration of supplemental screening or more frequent surveillance. The study also compared the AI tool’s discriminatory performance (AUCs) to established clinical risk calculators, such as the Tyrer-Cuzick and BCRAT models, and found that AI scores provided similar or better discrimination for short-term risk estimation.
However, it is critical to note that the AI algorithm did not “diagnose” cancer years in advance, but rather signaled increased risk based on image features. The study does not provide evidence that early AI-based risk identification directly leads to improved patient survival or reduced economic costs; such claims remain hypothetical and require further research.
Conclusions
This large, population-based study demonstrates that a commercial AI tool for breast cancer detection can identify subtle mammographic features years before a breast cancer diagnosis, supporting its potential role in risk-based screening strategies. Nevertheless, several limitations must be acknowledged: the retrospective design, evaluation of a single commercial AI algorithm, and the largely homogeneous (predominantly White) population. The authors emphasize the need for further validation in more diverse populations and prospective studies to determine the optimal clinical integration of AI-based risk assessment. Future research should aim to verify these results across diverse populations and effectively integrate AI risk assessments into standard clinical practice.
Journal reference:
- Gjesvik J, Moshina N, Lee CI, Miglioretti DL, Hofvind S. Artificial Intelligence Algorithm for Subclinical Breast Cancer Detection. JAMA Netw Open. 2024;7(10):e2437402, DOI: 10.1001/jamanetworkopen.2024.37402, https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2824353







 English (US) ·
English (US) ·